Back Pain During Pregnancy | Causes, Symptoms & Safe Relief Tips
-


Back pain during pregnancy is a common issue caused by hormonal changes, weight gain, and shifting posture as the body prepares for childbirth. These changes often put extra strain on the lower back and spine, leading to daily discomfort.
Back pain during pregnancy should always be managed under proper medical guidance from experienced pregnancy care specialists.
As pregnancy progresses, everyday activities like standing, sitting, or sleeping may become uncomfortable due to increased pressure on muscles and joints. Ignoring early signs of back discomfort can sometimes lead to reduced mobility and disturbed sleep. Understanding the causes of pregnancy-related back pain and adopting safe relief techniques at the right time can make a significant difference. Simple lifestyle adjustments, proper posture, and expert prenatal care help expecting mothers stay active, comfortable, and confident throughout their pregnancy journey.
At Silver Streak Multi Speciality Hospital, Gurgaon, pregnancy-related concerns such as back pain and posture discomfort are managed with expert medical guidance focused on both mother’s comfort and baby’s safety.
Dr. Swapnil Agrahari is an experienced Obstetrics & Gynecology consultant with 8+ years of clinical expertise and a 4.9★ rating from 2600+ patients. She is widely trusted for managing normal and high-risk pregnancies with a patient-centric and evidence-based approach.
She provides comprehensive pregnancy care, helping expecting mothers safely manage back pain, pelvic strain, and musculoskeletal discomfort through posture guidance, lifestyle support, and non-medicated relief methods. Her focus is always on reducing discomfort while maintaining overall pregnancy health. With advanced qualifications (MBBS, MS, F.MAS, D.MAS) and expertise in high-risk pregnancy care and minimally invasive gynecological procedures, Dr. Swapnil ensures personalised care and clear guidance at every stage of pregnancy.
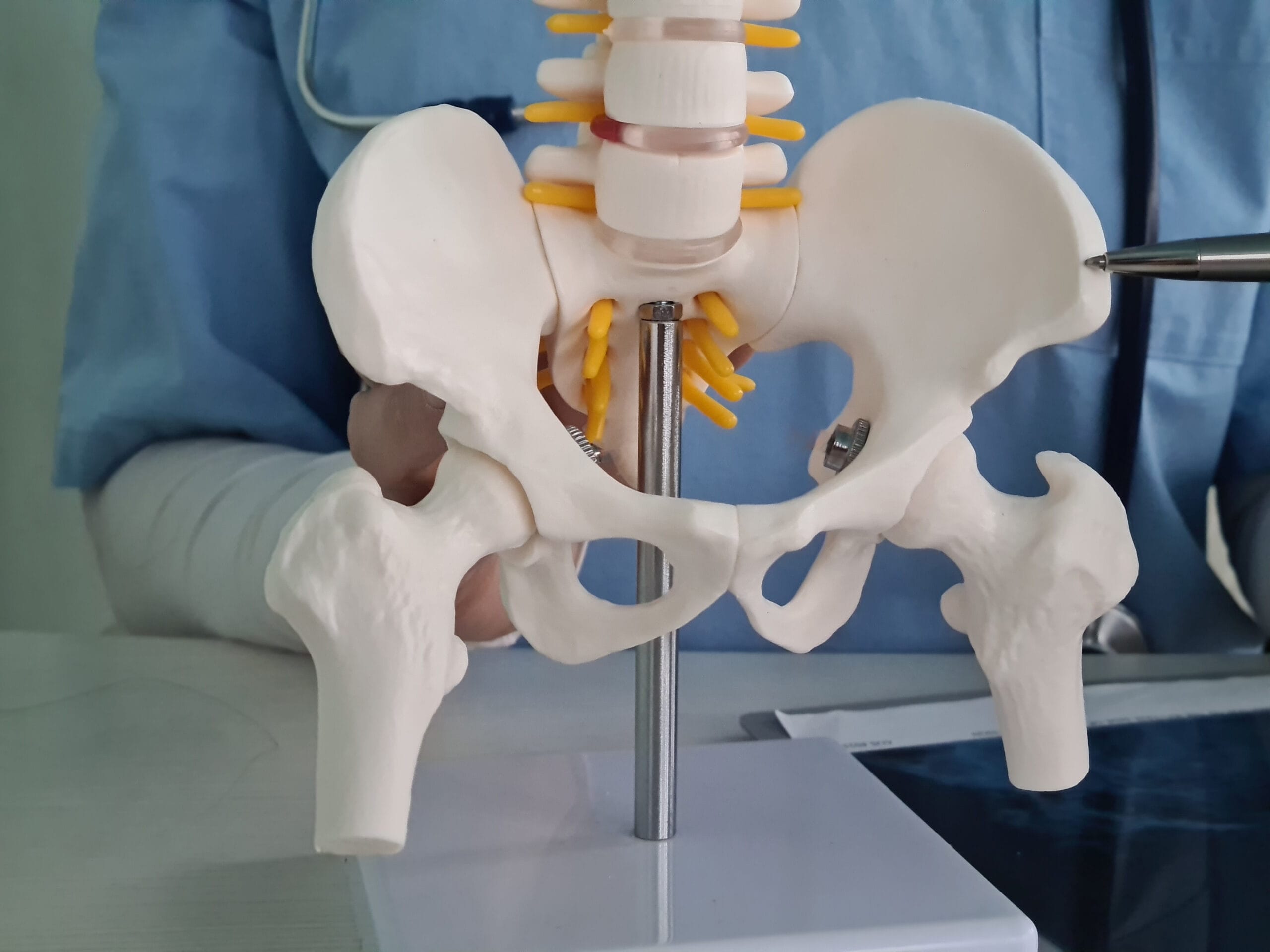
Back pain during pregnancy is a common concern and can appear at any stage as the body adjusts to support a growing baby. Hormonal changes, especially the release of relaxin, loosen ligaments and joints to prepare for childbirth, which can reduce spinal stability and lead to discomfort. Along with this, gradual weight gain, a shifting center of gravity, and posture changes increase pressure on the lower back, hips, and pelvic region. Pregnancy-related back pain may range from mild stiffness to sharp or persistent pain, often worsening after long periods of standing, sitting, or poor sleeping posture. In some cases, muscle fatigue, pelvic joint strain, or weak core muscles further contribute to discomfort—especially during the second and third trimesters.
1. Hormonal ligament relaxation affecting spinal support
2.Increased body weight placing stress on the lower back
3.Postural changes as the abdomen grows forward
4.Muscle imbalance and reduced core strength
5.Prolonged sitting, standing, or improper sleeping position
Gentle exercises & stretches: Prenatal yoga, walking, or simple stretches improve flexibility and strengthen supporting muscles. Maintain good posture: Standing tall, sitting with back support, and avoiding slouching can reduce strain on your spine. Sleep on your side: Use a pillow between your knees to align the spine and relieve lower back pressure.
Seek medical advice if you have., Severe or constant pain that doesn’t improve with rest or gentle movement. Numbness, tingling, or weakness in your legs, which may indicate nerve involvement. Pain accompanied by fever, abdominal discomfort, or burning urination, which could signal complications.
Back pain during pregnancy can often be managed with simple lifestyle changes and safe daily habits. In some cases, professional evaluation by back pain specialists helps identify posture or spine-related issues early. In some cases, professional evaluation by back pain specialists helps identify posture or spine-related issues early and prevents discomfort from worsening.
Gentle physical activity such as walking, prenatal stretching, or pregnancy-safe yoga helps strengthen the muscles that support the spine and improves flexibility. Maintaining correct posture while sitting, standing, and sleeping reduces unnecessary pressure on the lower back and pelvis. Using pregnancy pillows or maternity support belts can further improve comfort and spinal alignment.
In addition, relaxation techniques like deep breathing and short rest breaks help reduce muscle tension and stress, which often contribute to pain. When back pain becomes persistent or starts interfering with daily activities, seeking timely medical guidance ensures safe relief while protecting both the mother and the baby.
Gentle movement: Light walking, prenatal yoga, or stretching keeps muscles active and reduces stiffness.
Posture awareness: Standing and sitting straight helps reduce pressure on the lower back.
Supportive sleep: Sleeping on your side with a pillow between your knees supports spinal alignment.
Daily relaxation: Breathing exercises or short rest breaks calm muscles and reduces tension.
These natural methods are safe, effective, and recommended for most pregnant women.
Back pain can begin as early as the first trimester, although it is more commonly experienced during the second and third trimesters as physical changes become more noticeable. In early pregnancy, hormonal changes—especially the release of relaxin—start loosening ligaments and joints, which can reduce spinal stability and cause mild discomfort. As pregnancy progresses, gradual weight gain, a shifting center of gravity, and changes in posture place additional stress on the lower back, hips, and pelvic region. During the later months, the growing uterus and baby further increase pressure on muscles and nerves, making back pain more frequent or intense for some women.
The timing and severity of back pain vary from person to person. While some women experience only occasional stiffness, others may notice persistent discomfort, especially after standing, walking, or sleeping for long periods. Early awareness and supportive care can help manage symptoms effectively throughout pregnancy.
Pain relief during pregnancy must always prioritize the safety of both the mother and the developing baby. While discomfort such as back pain, pelvic pressure, or muscle strain is common, not all pain-relief methods are considered safe during pregnancy. Choosing the right approach is essential to avoid potential risks.
Non-medicated methods are the first and safest line of treatment for pregnancy-related pain. Gentle exercises such as prenatal yoga, walking, and guided stretching help strengthen muscles, improve posture, and reduce pressure on the spine. These activities also enhance blood circulation and reduce stiffness. Posture correction and ergonomic support play a key role in pain management. Using pregnancy pillows while sleeping, maintaining a straight posture while sitting, and avoiding prolonged standing can significantly ease back and hip pain. Maternity support belts are also effective in reducing strain on the lower back and pelvis. Heat therapy, such as applying a warm (not hot) compress to the affected area, can relax tight muscles and provide temporary relief. Warm showers are another safe and soothing option for muscle relaxation.
Among pain medications, paracetamol (acetaminophen) is generally considered safe when taken in the correct dosage and only under medical guidance. However, self-medication should be avoided, and prolonged or frequent use must be discussed with a healthcare provider.
Painkillers such as ibuprofen, aspirin, and other NSAIDs are usually not recommended, especially during the later stages of pregnancy, as they may pose risks to fetal development.
If pain is severe, persistent, or worsening despite lifestyle changes, consulting a gynecologist is essential. A specialist can identify the cause, recommend safe physiotherapy, or adjust treatment based on the trimester and overall pregnancy health.
Timely medical guidance ensures pain is managed effectively without compromising maternal comfort or baby’s safety, making pregnancy a healthier and more comfortable journey.
Yes, paracetamol (acetaminophen) is generally considered safe during pregnancy when taken in the recommended dosage and under medical guidance. It is commonly prescribed for mild to moderate pain, including back pain, headaches, fever, and body aches during pregnancy, as it does not interfere with fetal development when used correctly. Taking two paracetamol tablets (usually 500 mg each) at one time is often safe, but only if advised by a doctor or if it stays within the standard daily limit. The usual maximum recommended dose is no more than 4,000 mg in 24 hours, and doses should be spaced appropriately. Overuse or frequent intake without supervision should always be avoided.
Yes, gentle back massage is generally safe during pregnancy and can be an effective way to relieve muscle tension, stiffness, and lower back discomfort. As the body adjusts to hormonal changes, weight gain, and posture shifts, muscles around the spine and pelvis often become tight. A carefully performed massage helps improve blood circulation, relax strained muscles, and promote overall comfort without harming the mother or baby. It is important that pregnancy massage is done using light to moderate pressure only, especially in the lower back and hip area. Deep or forceful massage should be avoided, as certain pressure points may stimulate contractions. For best safety, massage should be performed by a trained prenatal massage therapist or under the guidance of a healthcare provider. Massage can be especially beneficial when combined with doctor-approved lifestyle measures such as posture correction, prenatal stretching, and adequate rest. However, if back pain is severe, persistent, or accompanied by symptoms like numbness, fever, or abdominal pain, medical evaluation should not be delayed.
When performed correctly, prenatal back massage offers a safe, drug-free pain relief option that supports both physical relaxation and emotional well-being throughout pregnancy.
A healthy morning routine during pregnancy sets the tone for the entire day by supporting physical comfort, emotional balance, and overall well-being. Starting the day slowly helps the body adjust to hormonal changes, reduces stiffness, and minimizes common discomforts such as back pain, fatigue, and nausea. Gentle stretching or pregnancy-safe movements after waking up can significantly reduce back and pelvic stiffness. Simple activities like slow neck rolls, seated stretches, or prenatal yoga poses improve blood circulation and prepare the muscles and joints for daily activities without putting strain on the body.
Hydration is essential first thing in the morning, as dehydration can worsen fatigue, headaches, and muscle cramps during pregnancy. Drinking a glass of warm water helps activate digestion and supports healthy blood flow, which is important for both the mother and the growing baby. Lastly, a calm and mindful start—such as deep breathing or a few moments of relaxation—helps manage stress and emotional changes common during pregnancy. A positive morning routine not only improves physical comfort but also contributes to better sleep, mood stability, and overall pregnancy health.
Crossing legs during pregnancy can reduce blood circulation and increase pressure on the pelvis and lower back.
It may also worsen swelling in the legs and contribute to poor posture. Sitting with feet flat on the floor and using back support helps maintain better spinal alignment and comfort.
Back pain during pregnancy is common, but it doesn’t have to control your daily life. With the right posture, gentle movement, safe pain relief methods, and a healthy routine, most women can manage pregnancy-related back pain effectively. Understanding when discomfort is normal and when medical advice is needed — ensures both maternal comfort and safety.
If you are experiencing persistent or severe back pain during pregnancy, consult experienced healthcare professionals for proper guidance and care. Early support can help you stay active, comfortable, and confident throughout your pregnancy journey.
1. Is back pain normal during pregnancy?
Yes, back pain is very common during pregnancy due to hormonal changes, weight gain, and posture shifts. In most cases, it is temporary and manageable with safe care.
2. Can back pain harm my baby?
No, mild to moderate back pain usually does not affect the baby. However, severe or sudden pain should always be checked by a doctor.
3. Which sleeping position is best for back pain during pregnancy?
Sleeping on your side with a pillow between your knees helps maintain spinal alignment and reduces pressure on the lower back.
4. Does walking help back pain in pregnancy?
Yes, gentle walking improves blood circulation, strengthens muscles, and helps reduce stiffness and back discomfort.
5. When should I worry about back pain during pregnancy?
You should consult a doctor if pain is severe, persistent, or associated with fever, numbness, abdominal pain, or difficulty walking.